Nanotechnology allows scientists to build better blood vessels
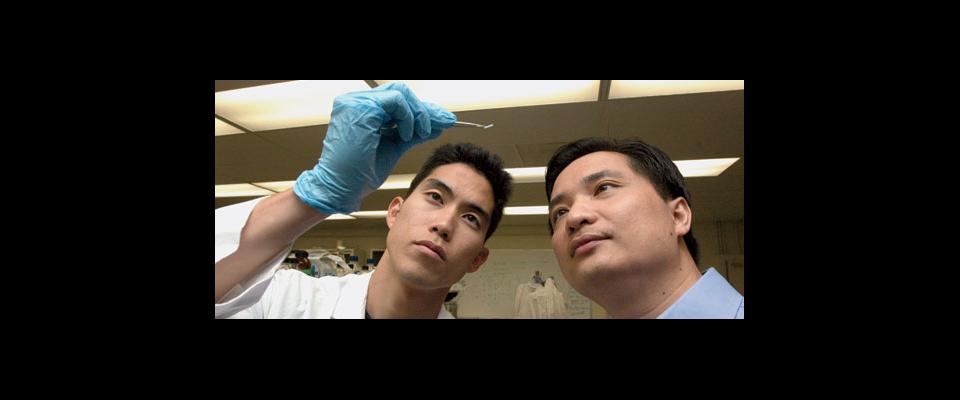
You could call Craig Hashi an interior designer, but he’s not designing the insides of homes or offices. His designs take shape within the human body, where he builds tiny, customized scaffolds shaped like blood vessels that, once implanted, help the body grow new arteries.
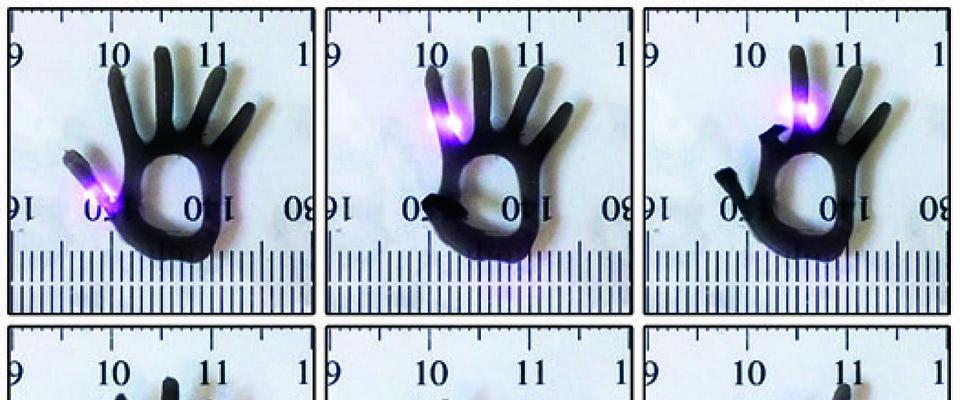
The Berkeley bioengineering Ph.D. student’s invention could eventually replace traditional coronary bypass surgery, the current treatment of choice for severe cases of heart disease. Each year, about half a million Americans undergo the procedure in which doctors typically remove a healthy blood vessel from the patient’s leg or arm and use it to build a detour around a blocked artery to restore blood flow to the heart. But these substitutes are far from perfect. Hashi and his team, led by bioengineering assistant professor Song Li, had a better idea: Instead of using second-hand replacement parts, why not help the body grow brand-new vessels out of its own tissue? The team developed so-called nanografts, tiny molds that can guide cells towards growing into new arteries. They started by creating very thin mats made of nanofibers and seeded them with adult bone marrow stem cells (in the trial, these were harvested from rats). The nanofibers mimic the native blood vessel tissue and “give the cells a more natural home to reside in,” Hashi says. After letting the cells grow for a couple of days, they carefully rolled the mat to form a tube, similar to the shape of an artery. Once implanted, the nanofiber tube degraded and left a fully-functioning blood vessel.
Their new procedure eliminates a host of problems associated with current procedures, Hashi explains. “The harvesting procedure of the replacement vein that is required in conventional coronary bypass surgery is extremely invasive and requires a second surgical procedure, which means a higher risk of mortality, higher hospital costs, and more injury to the patient,” he says. Some patients may not even have healthy, suitable veins or arteries, he adds. In such cases, doctors sometimes use synthetic arteries or transplants, but foreign material can be rejected by the body’s immune system. Hashi explains that his team’s technique would use the patient’s own stem cells, thereby reducing the chance of rejection by the host.
However, the procedure may not be risk-free. Some scientists have raised alarm at the rapid progress in the field of nanotechnology and warn that safety issues, such as the potential toxicity of nanostructured materials, will need to be sufficiently addressed.
Hashi and his team have tested their novel vessels with great success in rats and are hoping to move them to larger animals and then to clinical trials in the next couple of years. A patent for their procedure is pending, and with nearly 80 million baby boomers hitting retirement age over the next few decades, Hashi says the market can only grow.