As the death toll for COVID-19 crosses 100,000 people in the United States—the highest number of any country in the world—African Americans continue to be disproportionately impacted by the virus. Nationally, African Americans are nearly twice as likely to die from COVID-19 as would be expected based on their share of the population according to an NPR analysis. By contrast, in 37 states, whites make up a lower percentage of COVID-19 deaths than their percentage of the population. The trend holds in the Bay Area where, in the East Bay, cases have been heavily concentrated in Oakland, especially in East and West Oakland, where residents are disproportionately black and poor.
To understand why, California contributor Brandon Patterson talked to Tina Sacks, a professor at the UC Berkeley School of Social Welfare whose research focuses on poverty, inequality, and racial inequities in health. Sacks also previously worked on public health policy at the Centers for Disease Control & Prevention. The interview has been edited for length and clarity.
Around the country—including here in the Bay Area—black and Latinx folks have been hardest hit by the COVID-19 pandemic. In Alameda County, for example, the highest number of cases has occurred in Oakland—and in Oakland, they’ve been concentrated in East and West Oakland especially. What structural factors do you think account for this?
Tina Sacks: We see this pattern all across the country. The United States is built around structural inequality. Those things play out in terms of what’s happening with COVID because black people don’t have as many buffers. black people are not concentrated in jobs in which they can work from home. They’re also more likely to be in jobs that don’t have paid sick leave. They’re in public-facing jobs that bring them in contact with the public all the time like postal workers or a conductor on BART. That’s one big factor.

There are [also] other factors related to health. Black people have been systematically denied medical treatment for hundreds of years. They receive substandard medical treatment. Consequently, black people are much more likely to suffer from chronic health problems that make them more susceptible to COVID and dying from COVID. The conditions in which black people live and work are harmful to our health. Black people are much more likely to live in segregated communities that are fundamentally separate and unequal. They do not have the same institutional anchors that even lower income white communities have in terms of grocery stores, having some place to exercise, and fresh air. So black people’s health is really compromised at every level—and not to mention the psychic trauma that black people endure all the time in terms of police violence and day-to-day exposure to racism. The reasons are numerous but they’re really essentially the same across the country.
Can you say more about the historical lack of access to health care and pre-existing health disparities, and the role they plan in this pandemic?
TS: I’d put this into two different pockets. One is the conditions in the social world: Where you live. Where you work. What you’re exposed to. If you live next to a power plant. The kinds of stressors or inputs into your health and well-being. Black people are more likely to be exposed to things that are negative for health. Like toxic stress. Like environmental toxins. Like living in poverty. Having to work two jobs—not being able to sleep as much. Not having time to exercise. Having to care for multiple people in your family and therefore not being able to take care of yourself.
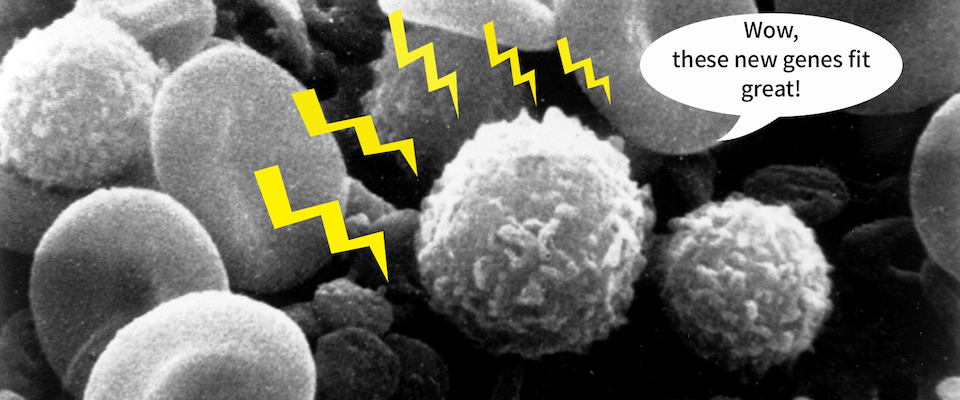
There are so many physical, environmental, and social stressors that make black people more likely to have these underlying conditions like diabetes, or asthma, or hypertension that make them more likely to be at risk for COVID and fatalities related to COVID. People often talk about race as a risk factor for illnesses, including COVID. It is not race that is a risk factor—it is racism that is a risk factor. It’s not that black people are genetically predisposed to have all of these illnesses. It’s the lifetime of exposure to structural discrimination as well as the intergenerational transfer of the consequences of that discrimination.
Black people [also] have always had a very fraught relationship with predominantly white healthcare institutions and for very good reason. For a long time they were not able to access care. There is a long history of experimentation on black people. We’re also hearing many cases of black people during the pandemic who presented in emergency rooms only to be turned away two or three times. Black people’s complaints are often not taken seriously and black people die as a result. This is part of a much larger problem that we face as a country. It’s not just about COVID. What’s happening with COVID is really laying bare the underlying problems in the United States.
In a recent poll, only 25 percent of black people said that they would get a COVID vaccine when one becomes available, compared to 32 percent of Latinx people and 62 percent of white people. That’s despite the fact that black people are being hit the hardest. Why do you think that is?
TS: I’m not surprised by that. The most obvious example of malfeasance in the medical system is the Tuskegee syphilis study, which people point to all the time to explain why black people are reticent to engage in biomedical research, to take new treatments. Tuskegee is an illustration of a much broader pattern. So the fact that black people are reticent to take this vaccine can be due to this fundamental mistrust. I have heard some people say, ‘Well, let white people get it first and then we’ll see. If it’s going to be okay for white people then maybe we’ll do it.’ So there’s a level of vigilance that you wouldn’t see with white Americans, perhaps.
Some African American men have expressed hesitance about wearing masks in public due to fear of being targeted by police. How does that relate to how this pandemic manifests in black communities?
TS: Policing is a form of social control. It’s a way of controlling black people in a public space. So this is just another extension of the kind of brutality and diminishment of black humanity that we see across the board. I think it makes a huge difference when you see that a lot of black people don’t want to go outside in a mask and be a target for police. The point of wearing a mask is to try to protect all of us. So if black people are afraid of wearing a mask because they might be targeted by police, that could inadvertently lead to more spread of the disease.
What kinds of policies are needed to address COVID and related inequality long term?
TS: I often think about social policies that could have mitigated this whole situation. We need rational social policy. We need paid sick leave. We need universal health insurance. We need people to be able to get the kind of care they need without fear of what it’s going to cost or what happens if they don’t go to work. Most other industrialized countries have these kinds of policies. The United States has resisted them at every turn. We are one of the only countries in the industrialized world that does not have any kind of child care. We need housing subsidies. We need a social safety net that actually makes sense. Research has shown that countries that invest in housing, health insurance, education, and child care have much better health outcomes. Because those are the things that matter in the long run. And they’re not separate from the implications of COVID.