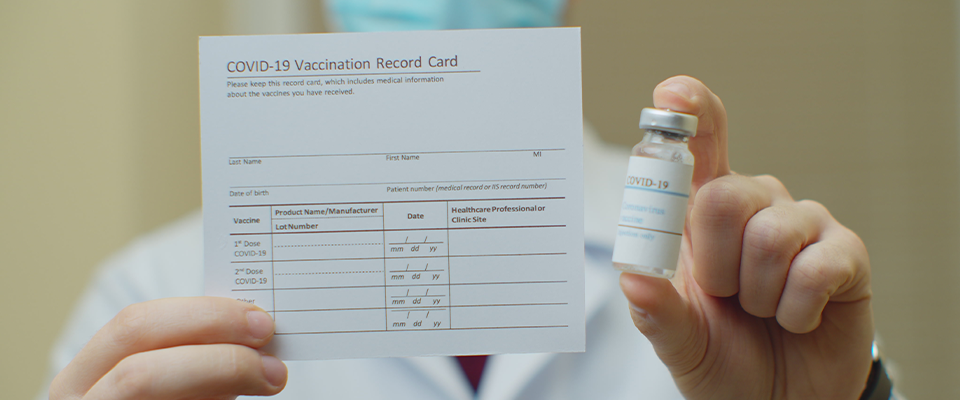
We’re well into the COVID vaccine rollout, and if you have more questions than ever, you’re not alone.
On Monday, March 15, Berkeley Events and the UC Berkeley School of Public Health invited four experts to a virtual public forum to discuss the ongoing vaccination strategy, focusing especially on questions of vaccine access, safety, and the results we’re seeing so far.
“Community members of all racial backgrounds have concerns about whether scientific developments in medicine are safe to use.” —Osagie Obasogie
It turns out there’s much to celebrate. Dr. Erica Pan, who is California’s state epidemiologist and the deputy director of the Center for Infectious Diseases started the discussion by emphasizing that when California made the call to initiate a state-wide lock-down almost exactly a year ago, neither she nor her colleagues imagined that a vaccine with a 90 percent efficacy rate would be developed by the end of December.
California’s vaccination rate is on a par with other large states, with over 14 million people having received the vaccine. Dr. Pan also said that California has been successful in meeting various equity benchmarks with regards to vaccine rollout, like setting aside 40 percent of available doses for neighborhoods that have been hardest-hit by the virus, most of which are clustered in the Central Valley and Los Angeles county.
Dr. Arthur Reingold, a professor at the School of Public Health, was similarly complimentary of distribution efforts nation-wide, although he thinks it’s “remarkable we’re doing as well as we are,” given that “political pressures have driven a constantly evolving set of priorities about who should get vaccinated before someone else.”
For many, Dr. Reingold’s point about triage hits on some fundamental, and perhaps unanswerable, questions: Why are some people who want the vaccine having trouble getting it? Who should be getting it, and when? What about people who don’t want to take the vaccine?
Bioethics professor and Haas Distinguished Chair Osagie Obasogie said that a shift is due in the way we frame the public conversation about vaccine hesitancy. We’ve been hearing for months now that African American communities might be more hesitant to take the vaccine because of historical memories of medical malpractice, like the Tuskegee Medical Trial, but Obasagie says that more recent studies are showing that reports of vaccine hesitancy in Black communities are overblown, if not simply false. For example, 73 percent of Black people say they plan to get the vaccine or have already, while only 70 percent of white people say the same.
“Many community members of all racial backgrounds have concerns about whether scientific developments in medicine are safe to use. Black people have the same capacity as anyone else to make informed decisions about vaccines,” he said.
“Vaccine access for people that are disabled and housebound is going to be different to vaccine access for people who are able-bodied and going to Whole Foods.” —Dr. Colette Auerswald
Dr. Colette Auerswald, an associate professor at the School of Public Health who specializes in adolescent and community health, added that politicians and public health officials should prioritize development of more than one vaccine plan to fit the needs and abilities of all Americans, especially those who have been pushed to the margins of society.
“We need vaccine plans that fit all the different intersectional identities of folks and all the different types of lived experiences,” she said. “Vaccine access for people that are disabled and housebound is going to be different to vaccine access for people who are able-bodied and going to Whole Foods, and that’s different from folks in rural areas and depending on clinics that aren’t open right now.”
What does that actually look like in terms of policy and implementation? For Dr. Pan, a step in the right direction is finding trusted leaders in small communities and providing them with the tools and resources to ensure that people with less access to vaccine information know when and where they can get vaccinated. It also means prioritizing vaccination for people who fall into the lowest quartile of California’s Covid Healthy Places Index, a database that takes into account metrics like access to transportation, housing, education, and healthcare.
Everyone agreed that a lack of long-term data on the vaccine’s side effects shouldn’t deter people from getting it. Historically, the unwanted side-effects of every new vaccine have developed within eight weeks of the vaccine being administered. By that metric, current COVID-19 vaccines are safe—though any new vaccine or medication carries some long-term uncertainty. Still, the panelists agreed that the benefits of being vaccinated “far, far outweigh” the risks of forgoing the jab.
A much-reiterated take-away from the panel was the necessity of reframing how we think about public health in this country. Until now, said Professor Osagie Obasagie, many people have thought (and some continue to think) of public health on too small of a scale, focusing on individuals, rather than communities.
Even in the coming years, patience and cooperation will continue to be important as new virus variants develop, necessitating booster shots and updated vaccines.
Infrastructure needs to change, too, both to speed up our response to this pandemic and to better prepare for the future. “Public health has single-handedly kept the fax industry alive,” Dr. Pan quipped. “That’s a big part of why we don’t have good data. We’ve been saying that you need to invest in advance in health and public health – hopefully this time we’ll listen.”
Dr. Reingold agreed that there are lessons to be learned: we need better coordination and we need better medical infrastructure, like up-to-date, searchable registries. He was less optimistic that people would heed the lessons. “I’m far and away the oldest person on this panel,” he said, “and what I would say is we’ve once again relearned a lot of lessons, none of them new.”
So what can we expect in the coming months—and years? Most panelists were reluctant to play the role of fortune-teller but agreed that teenagers—one of the lowest priority groups for vaccines in California and most of the country—would likely become eligible for vaccines in California before school starts in the fall. Several also remarked that COVID vaccination might very well become a requisite for activities like university attendance and workplace participation across the country. The idea of a “COVID passport” might sound controversial, but Dr. Reingold insisted it’s nothing new; schools, including UC Berkeley have long required students to be immunized against measles, for example.
Even in the coming years, added Dr. Pan, patience and cooperation will continue to be important as new virus variants develop, necessitating booster shots and updated vaccines. “I see this as a vaccine-preventable disease,” she said. At the same time, she doesn’t see it going away. “It’s way too smart. We haven’t been able to get rid of the flu, and this is a much smarter virus.”