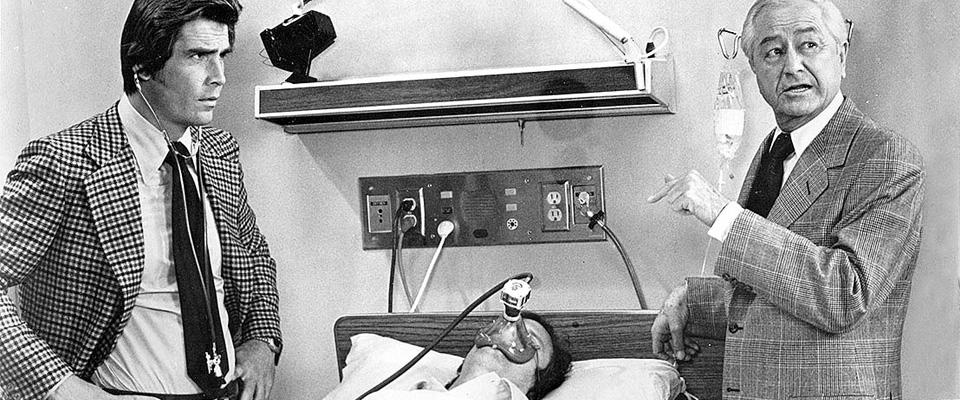
After her second above-the-knee amputation, Ms. G., a 56-year-old woman with diabetes mellitus, started refusing her dialysis and wouldn’t tell the medical team why. Jodi Halpern, hen just a trainee on the psychiatric service, was sent to investigate. On entering the hospital room, Halpern recalls finding the woman in agonizing pain. When Halpern sat down to talk to her, Ms. G. eventually opened up and explained that her husband was divorcing her because he no longer loved her after her amputations. Halpern recalls explaining to her supervisors that Ms. G. was emotionally distraught and not rational. They advised her to remain professional and objective and not to get involved.
Ms. G. died soon after, and Halpern never forgot—that case became the foundation of her seminal work, From Detached Concern to Empathy: Humanizing Medical Practice, first released in 2001 and recently reissued in paperback. Now a medical doctor, psychologist, and UC Berkeley professor of bioethics, she has become an expert on the role of empathy in medicine. In a recent perspective she co-authored for World Psychiatry, she criticized the medical tradition of adopting “detached concern” when dealing with patients. Halpern believes medical schools “need to stop un-teaching” empathy.
Most patients, of course, would prefer to receive care from a doctor with a compassionate bedside manner, but Halpern suggests that the effect of better empathic listening skills could be huge. Currently, an estimated half of all patients don’t take the medications they’re prescribed as directed. This may result from poor communication, the patients’ lack of trust in the doctor, or reluctance to discuss embarrassing side effects, such as the sexual dysfunction that can accompany certain blood pressure medications. But drawing from her own experience in the field, Halpern says that when doctors really listen and show they care, patients are more likely to open up.
What’s more, doctors would likely benefit from being more empathetic. In her paper, Halpern wrote that many people start medical school with a high level of empathy, but studies show that, not surprisingly, they become less empathetic as they suffer burnout. Although the cause of burnout is complicated, contributing factors likely include stress, fatigue, and an environment that teaches objectification of the patient. Halpern says that medical training should include more emotional support for trainees and new doctors to allow them to relax and act, well, more human. Even a simple technique like deep breathing could help them “be present” when interacting with their patients and enjoy the very reason they got into the medical field—helping people feel better.
She argues that doctors need to be more curious about their patients, instead of assuming they already know what patients are going through. “We need to recognize that each person is a world, and a complex one, and we never know the complexity of what they’re feeling.”