The future will be an exciting time to be alive, if for no other reason than it will be so much easier to survive.
We’ll have a bewildering variety of replacement parts for our organs and limbs. Stubborn diseases will be tamed by exotic treatments. New technologies will enable not just better living, but new ways of living. And the human body will reveal all of its secrets in response to our probings in… (dramatic pause) … the year 2000.
Here are, according to the scientists and futurists polled by Time magazine in 1966, just a few of the miracles we should have already experienced before Wi-Fi became available in most coffee shops:
• Artificial hearts, lungs, and stomachs
• Artificial skin, complete with noses and ears
• Mechanical limbs guided by our brains
• Fetuses grown in artificial wombs, the ultimate labor-saving device
• The blind shall see and the deaf hear
• Anti-grouch pills and ambition pills
• “Nearly all experts agree that bacterial and viral diseases will have been virtually wiped out”
• “Probably” a cure for arteriosclerosis
Woof. The future is hard.
If you’re keeping score, by 2000 we had achieved artificial hearts, cochlear implants for the deaf, and Prozac. By that time, we’d also seen the rise of antibiotic-resistant superbugs and the HIV/AIDS epidemic. Heart disease remained, then as now, the leading cause of death in the developed world—and few foresee the imminent demise of bacterial, viral, or heart diseases.
But the rest of the stuff? Intelligent mechanical limbs, new sheets of skin, and custom-grown organs? All of that and so much more seems closer than ever. Probably. Maybe. We hope.
When it comes to rebuilding the human body, the hard stuff is the easy stuff. That’s to say that for quite a while now it’s been easier to repair a body’s mechanical deficiencies than its biological failings. For 50 years, we’ve been replacing hip and knee joints with a combination of metal, plastics, and bone cement. Heck, each year more Americans have a hip replaced than their appendix removed.
The easiest prediction to make about the future of medicine is that we’ll manufacture even better replacement parts for ourselves. New technologies such as 3D printing can make parts based on medical imaging and customized to individual patients. We’re already seeing the first of these parts being put into humans.
But maybe you’re just not impressed with the mechanical wizardry. After a couple of decades of hearing about DNA this and stem cell that, you want the good stuff. You want replacement parts made from living tissue, preferably human, preferably brand-new, and preferably yours—none of those used parts from teenage motorcyclists. Only new and bespoke human tissue, please.
Look, building a functional organ will require a billion or more cells, and they’re not all the same type of cells. They’re not even facing the same way. You have to build structures of different cells, all correctly oriented and connected. And you can’t just pile them on top of one another; there has to be vasculature so they can take in nutrients and expel waste, all of them, all of the time. It’s the difference between pouring a concrete floor and building an apartment tower. Scientists are, in fact, making progress. But Rome wasn’t built in a day, and neither is a liver.
So if you’re wondering when you can pick up your very own replacement liver and kidneys in order to shrug off the pleasures of a hedonistic youth, here is one definite bet about the future of medicine. A cool fiver laid down on the felt table of history: Science will build you a new sphincter before it makes you a replacement booze filter.
Plan your remaining years accordingly.
Herewith, a brief tour of some of the latest and most intriguing medical developments, some already on the market, others on the horizon–or so we hope.

In 2013, the FDA approved 3D- printed plastic skull and facial implants made by Oxford Performance materials, a Connecticut company. Shortly thereafter, a patient in the northeast had 75 percent of his skull replaced with a gray biocompatible plastic called PEKK. Not only is the material similar to bone in its density and strength, but it’s perforated with small holes to allow the patient’s own bone cells to grow and attach to it. Being plastic, it’s safe in a CT scanner and only shows up as a shadow in X-rays. Alternatively, in 2014, Dutch doctors at University Medical Center Utrecht replaced the entire top of a woman’s skull with a 3D-printed acrylic implant from an Australian company. The implant was entirely clear, enabling surgeons to watch out for fluids or hematomas. The 23-hour surgery was a success, her scalp was replaced and, doctors say, there’s little trace at all of the surgery—which is undoubtedly for the best, but my God, can you imagine how much fun a see-through skull would be at parties?
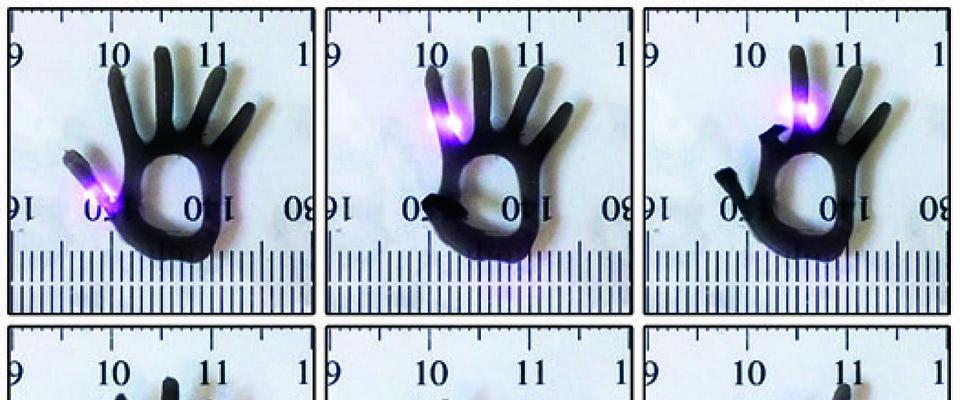
Twice since 2012, doctors at the University of Michigan have printed custom splints to surround the airways of infants with weakened tracheae and bronchi. In its milder forms, this weakening can be mistaken for asthma, but in severe cases it’s a life-threatening condition that requires the child to be placed on a respirator. The splints, though, allowed these babies to be weaned off the devices and are flexible enough that they will grow with the patient. They are printed of a material that will dissolve safely within three years, by which time the children’s tracheae should be robust enough to function on their own.
Available in the United States since 2013 is the Argus II, better known to the public as the bionic eye. Developed by a Southern California company called Second Sight, the device uses a small video camera attached to a pair of Terminator-worthy sunglasses to capture the scene in front of the user, which is then processed through a wearable computer and fed into an antenna mounted on the eyeglasses. The information is broadcast to an implanted array of electrodes in the user’s eye, where it is delivered as a series of electrical pulses through the undamaged portion of the retina to the optic nerve. For this to work, the patient has to suffer from the most common kind of inherited blindness, retinitis pigmentosa, which robs him of the ability to see light but otherwise leaves his retinas intact. What the Argus can restore for these people is not yet the ability to read a book or drive a car, but to see a world of 60 black-and-white pixels. That’s enough for patients to track movement, follow a line, perceive a doorway, and see people in front of them. By 2017, Second Sight hopes to begin human trials for a new model of implant that would bypass the retina and the optic nerve and communicate directly with the visual cortex. If successful, that would mean nearly all forms of blindness could be treated with a bionic eye.
Researchers at Wake Forest Institute for Regenerative Medicine in North Carolina are working with the military on an inkjet-style printer that sprays layers of skin cells directly into wounds. So far, Wake Forest has had success printing large swaths of skin gel into fresh wounds on the backs of (heavily anesthetized) pigs, where it has cut healing time almost in half. Wake Forest say it hopes to have this technology ready for soldiers within five years. The military is especially interested in using it to give burned soldiers new, natural-looking skin complete with sweat glands, pigment, and hair—an estimated 8 to 20 years off.
This spring, UC Berkeley researchers led by Professor Kevin Healy, chair of the Department of Bioengineering, announced that they’d developed a three-dimensional strip of pulsating human heart tissue embedded on a silicon chip. The living tissue was grown from adult stem cells and coaxed into forming a model of a heart’s connective tissue and surrounded with tiny channels that would allow it to be exposed to drugs and nutrients in the same manner as it would if it were in a fully grown organ. This “heart-on-a-chip” was funded by the National Institutes of Health, which is seeking to develop a whole range of similar miniature organs to reduce the cost and increase the speed and accuracy of preclinical drug testing.

Ekso Bionics is a startup out of the Berkeley Robotics & Human Engineering Laboratory led by Professor Homayoon Kazerooni. As its name suggests, the company builds motorized exoskeletons for humans. Their flagship product, the eponymous Ekso, is an adjustable suit of bionics worn over clothing. It works for anyone with lower-limb disability, allowing them to make themselves walk using buttons on two crutches that come with the Ekso. One prototype of the device helped paralyzed Berkeley student Austin Whitney walk across a graduation stage in 2011. Nathan Harding, CEO of the company, got his master’s degree in mechanical engineering at Berkeley in 1993, and then worked as a consultant in the Robotics & Human Engineering Laboratory where the Ekso’s technology was developed. “I think there’s a giant wave of human augmentation coming for the human race…. It’s already started with devices such as hearing aids, and now you’ll see devices that allow us to run faster and jump higher.” The current Ekso is used in physical therapy and since 2012, the company has sold or rented more than 125 to clinics and hospitals. Ekso Bionics is also partnered with Lockheed Martin to develop load-carrying bionics for infantry soldiers. And the company is working directly with the U.S. Special Operations Command on a combat suit project called TALOS, which Harding says is their “program to get as close to Iron Man as possible.”
The laboratory-grown replacement part that seems most likely to make it to patients first is bone grafts grown from a patient’s own genetic material. A New York–based company called EpiBone has a promising process. They start with a CT scan to model a damaged segment of bone. From that, they create a scaffold by milling down a bit of cow bone that’s stripped of its own cells. They then seed the scaffold with a sample of the patient’s adult stem cells. The scaffold and the stem cells are then put in a bioreactor—basically a 3D-printed mold of the bone’s final shape—and a nutrient bath is pumped over it for three weeks to grow the bone. So far, EpiBone is implanting facial bones into pigs, but the company has told the press it hopes to be in FDA human trials within the next three years.
A major complaint and embarrassment for the elderly is incontinence—it’s no great thing to have survived life’s trials only to be let down by your own fundament. It should be some comfort, then, to know that Khalil Bitar, a professor at Wake Forest School of Medicine, has been developing an internal anal sphincter bioengineered out of circular smooth muscle cells and enteric neuronal progenitor cells. Human cells, mind you. The lab-grown sphincters have been implanted in rats lacking thymus glands (they thus do not reject foreign cells). Post-mortem examination of the sphincters revealed that they had formed vascular connections to their hosts and retained nervous function. Even more importantly, when the rats were still alive, researchers observed normal stooling.

Of course, most of us won’t, we hope, lose an organ or need a replacement limb. We’ll just get creakier as our bodies wear down and get slower in thought as our brains grow fewer neurons. You may have already noticed this in your own life, perhaps while trying to open a childproof bottle of painkillers or while wondering why anyone would need a new piece of beeping and incomprehensible technology when papyrus scrolls are still readable. And so what most of us could use, besides some fiber and a nap, is a pill to halt aging or, better yet, reverse it. And that’s why it’s so heartening to learn that scientists at the Berkeley Stem Cell Center have just this spring tested in mice a drug that appears to do just that. Specifically, there’s a growth factor called TGF-beta1 that increases as we age and inhibits the ability of our stem cells to generate new muscle and brain tissue. The researchers’ drug knocks down TGF-beta1 levels, and the old mice grow new brain tissue at a youthful level. The bad news, though, is that TGF-beta1 is just one part of the biochemical process of aging, and what we’ll ultimately need is a combination therapy of different drugs in carefully calibrated dosages. And, as always, it’s a long ways from lab rats to people. For the foreseeable future, we’ll likely still grow old the old-fashioned way. Dammit.
Brendan Buhler is a freelance writer and stay-at-home chicken keeper. He is a frequent contributor to California.