Two years into the pandemic, SARS-CoV-2 continues to defy predictions. At the date of this writing, the Omicron variant—as contagious as ultra-transmissible viruses such as measles, if somewhat less severe than earlier COVID variants—continues to spread rapidly. While the surge appears to be ebbing in some areas of the United States, hospitalizations remain high and, nationally, about 2,500 deaths are reported daily.
While the pandemic has affected every sector of society, none have been under more pressure than those in medicine and public health. Practitioners have endured high risk of infection and long shifts under crisis circumstances while public health authorities, as the bearers of bad news and champions of often unwelcome measures, have had to withstand denunciations and even death threats.
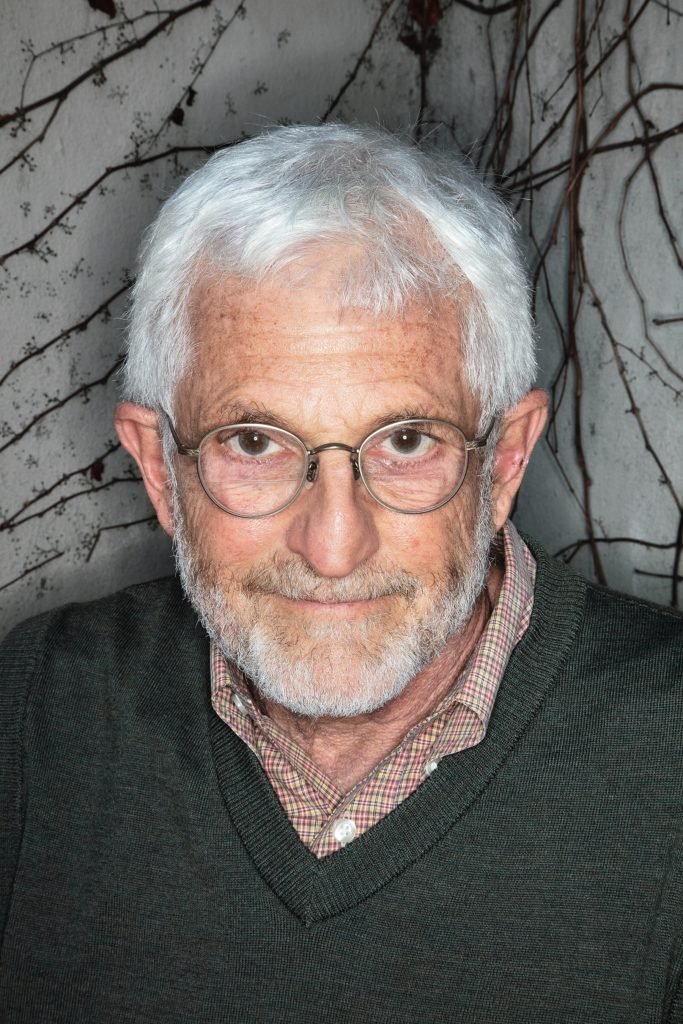
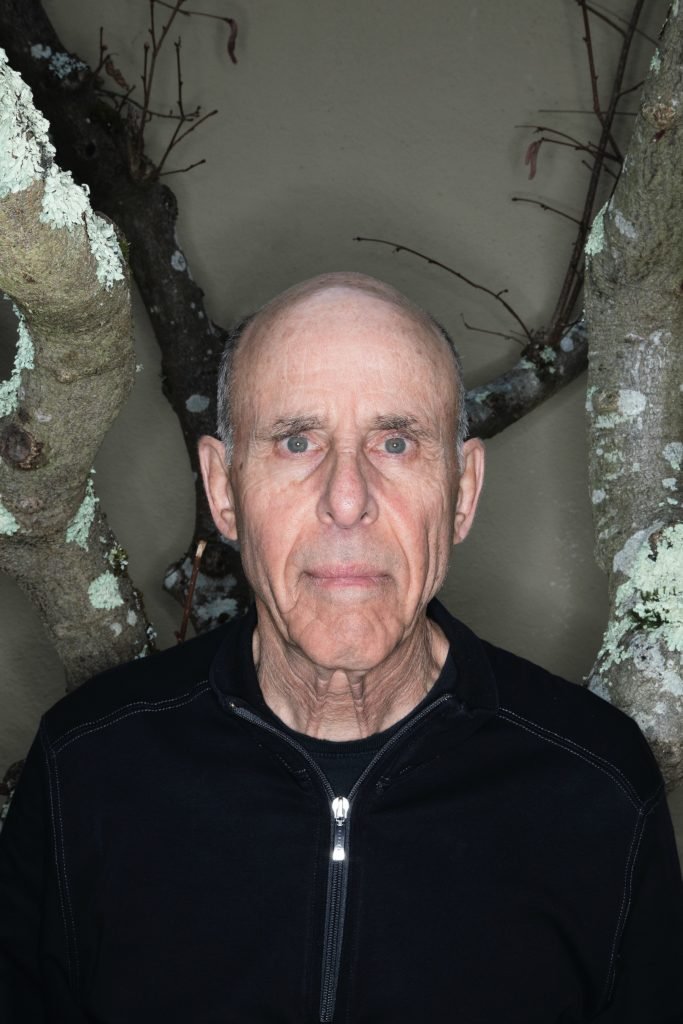
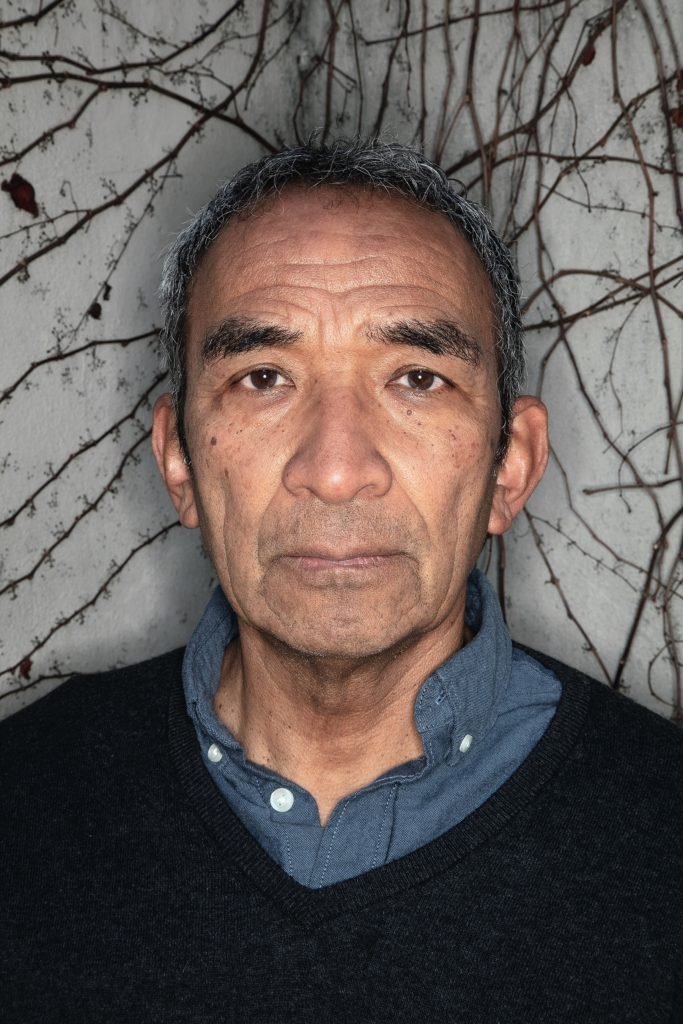
So how, we wondered, are epidemiologists and infectious disease specialists holding up, and what are they thinking at this point in the planet’s most serious infectious disease outbreak since the influenza of 1918? To find out, California contributor Glen Martin talked via Zoom with three of Berkeley’s leading public health experts: Arthur Reingold, professor of epidemiology; Lee Riley, professor of epidemiology and infectious diseases; and John Swartzberg, a clinical professor emeritus in infectious diseases and vaccinology.
This interview has been edited for length and clarity.
This pandemic has been long and arduous for everyone and, given your professions, you’ve been in the thick of it. In some ways, your role seems analogous to that of career military officers during wartime. What has the experience been like for you?
Reingold: If you use that analogy of a career military officer, your reaction would depend on whether you’re 35 and at the beginning of your career or 65 and near the end. For someone who was sort of hoping to glide into oblivion, well, it’s kept me busier than I thought I would be at this stage of life.
Swartzberg: It’s been a full-time job, and it’s been both exhilarating and depressing. You know, our careers have been bookended by public health crises. The first was in the early ’80s, with HIV. And now my career appears to be concluding with SARS-CoV-2.
Can you characterize the differences between those two health crises—AIDS and COVID-19?
Reingold: Well, obviously, for HIV there’s a very long incubation or latency period. AIDS takes years to develop, while it’s a matter of days with COVID, so things unfold in a very different time frame. Clearly, the public health response to COVID has been more rapid.
Swartzberg: But interestingly, public health in general was a more robust institution [at the advent of the HIV epidemic].
Reingold: Quite right. Over the past 20 years, there has been a steady erosion in the capabilities of state and local health departments.
Swartzberg: But there were similarities in the political response. Reagan wouldn’t even mention the acronym AIDS until his second term. And now we’ve seen this bizarre politicization of an infectious disease that defies all rational thinking. COVID came at a time when our society was already split, and [the virus] has just aggravated that to no end and for no good reason.
And psychologically for me, as a clinician, AIDS and COVID have been very different. I was a lot younger during the AIDS epidemic, and while there are real stresses when you’re taking care of patients, it didn’t feel very threatening to me personally. I felt more invincible than I do now in my mid-seventies. Now, I wonder every time I go out the door, “Am I going to get infected today?”
Dr. Anthony Fauci has endured ongoing ad hominem attacks and even death threats throughout the pandemic, and other public health officials have also been harassed and threatened. Could you share any thoughts on that, and have you encountered similar abuse?
Riley: It’s really sad to see that kind of animosity, but I think it’s a small segment of the U.S. population that’s responding this way. I haven’t experienced any hostility, but I know some of my colleagues have had issues.
Swartzberg: I’ve gotten maybe a dozen or so emails that were threatening—some very threatening. Some were anti-Semitic. That’s been about the extent of it.
Reingold: The only thing I’ve faced along those lines was about 15 years ago. I had a brilliant student who firmly believed vaccines cause autism, and he took great exception to my views to the contrary. He was in fact manic-depressive and unmedicated. He had a psychotic break, and he went to my office during office hours with a large hammer, presumably intending me bodily harm. The one mistake he made was assuming a Berkeley professor would be in his office during office hours. [Laughs.] I happened to have been in Geneva. I like to say it’s one of the few times that a meeting in Geneva saved a life.
So, no, I’ve never experienced anything like what my colleagues in local public health have experienced, which is very upsetting. Unlike the guy who intended me harm, most people protesting outside officials’ homes or sending threatening emails don’t have a psychiatric diagnosis; they just have a very different understanding of life than I do.
Have you arrived at any kind of sympathy for, or understanding of, that worldview?
Reingold: The quick answer is “no.”
The virus itself has considerable say in this. It is selecting and will continue to select unvaccinated people.”
Lee riley
Swartzberg: For years, I’ve taught a class on vaccine hesitancy in which we try to wrap our heads around it. We have people like Art and Lee as guest lecturers. We have anthropologists, philosophers, English professors, and really, the whole university community coming at it from multiple directions. And after several years of teaching this class, it’s still a very tough nut to crack. And I think that’s because there are multiple reasons people have for resisting vaccines.
Riley: There has always been a certain resistance to vaccines and modern medicine generally, but I think it’s really been exacerbated by social media. Before we had the internet, you couldn’t disseminate misinformation at anything close to the current scale. To really be responsive to these kinds of pandemics, we need to change the culture. I’m not advocating an autocratic government to enforce policy, of course, but you can’t just be completely individualistic. You have to be mindful of other people. Individualism is good in certain situations, but in terms of pandemics and public health, it can result in widespread infections, hospitalizations, and deaths.
But the virus itself has considerable say in this. It is selecting and will continue to select unvaccinated people.
Reingold: One of the things I’ve found particularly distressing is debates I’ve had with [some members of] the California Nurses Association around mandatory influenza vaccination for health care providers. Many nurses violently object to mandatory vaccination. My point is that education is not the only issue. It may be part of the issue, but in terms of the general population, we are never going to achieve a higher level of biological and medical education than exists among nurses. Yet many remain adamantly opposed. I can argue with them until I’m blue in the face, and it doesn’t change anything. I find that really depressing.
One achievement from this pandemic has been the rapid development and deployment of effective mRNA vaccines. How significant is that?
Riley: It’s the biggest development in vaccines we’ve seen in a very long time, although it didn’t start with SARS-CoV-2. An mRNA vaccine had been developed against Ebola during the last big outbreak, in fact, but by the time they were ready to do clinical trials, [the epidemic] had largely disappeared, so they could never demonstrate efficacy. But our experience with the COVID vaccines shows they’re safe and highly effective.
Reingold: It may well revolutionize vaccine production, and I hope that people resisting the COVID vaccines will lose their fear because at the moment, some say the reason they’re afraid of them is because they’re produced by “new” technology.
Swartzberg: The most important advance in the biological sciences in many years is CRISPR, but I’d put mRNA vaccines right up there. We’ve been working [with mRNA vaccines] for quite a long time, and it was fortuitous that it all came to fruition at the same time as the pandemic. There was a recent paper in the New England Journal of Medicine about developing a pan-coronavirus vaccine [which could include cold viruses] with mRNA technology. And what about a pan-influenza vaccine? Both possibilities are very realistic, and people are working on them right now. So, yes, it is huge.
Riley: And there are many other mRNA vaccines we’re thinking about, including one for urinary tract infections, which currently is the most common bacterial infection among women. One thing with the COVID pandemic and mRNA vaccines: We somehow got focused on the concept that two doses would be all we needed. And there was some confusion and maybe resentment when the booster was recommended later. I think we’re going to have to approach this as we do influenza. It’s likely we’ll need to be vaccinated annually, or maybe even semi-annually. It all depends on the severity of the epidemic. That’s going to be the norm, I think, and we’re just going to have to accept the concept that there’s not going to be any “right” vaccine dose.
One of the things they teach in medical school is that you are not the patient—you need to maintain a certain emotional distance to treat serious illnesses and injuries. Has that concept applied to your experience with this pandemic?
Reingold: Well, I left clinical medicine after finishing my residency and went into public health because I just found clinical medicine too depressing. Treating a 35-year-old woman dying of breast cancer, or a 16-year-old boy with lymphoma—it was just very difficult emotionally, and I was far more comfortable in public health and prevention, where we’re operating at population levels.
Riley: Like Art, I’m in public health rather than the clinical side these days, and I haven’t seen patients in many years. But even those of us in research and teaching have seen some burnout, particularly among the older faculty. Some of us are reluctant to accommodate in-person teaching, either due to personal concerns or concern for the health of family members. There’s also the frustration caused by not being able to teach in-person because that’s our profession; it’s something we take pride in and enjoy.
I also run a laboratory research group, and the shutdowns and gradual reopenings have been very stressful for my students. Their work and research have really been set back by all of this. These people need to graduate and get their Ph.D.s, and get out there and work, and the pandemic has hindered all that and put a great deal of strain on them.
For that matter, I’ve been stressed by the supply chain impacts the pandemic has imposed. It now takes many months just to obtain simple things we need for research.
Swartzberg: Having had a foot in both sides, public health and clinical medicine, I’m glad I’m in public health right now. As Art says, it’s more comfortable to sit back and think about things rather than confront the crisis directly on a day-to-day basis.
Has the pandemic taught us any lessons that will make our public health response stronger going forward?
Swartzberg: We’ve clearly learned that we’ve underfunded public health for too long. We need to stop thinking in terms of five-year packages for our public health infrastructure and demand robust funding on a continual basis. We can’t afford short-term thinking, given we’re dealing with SARS-CoV-2 now, and could very well face SARS-CoV-3, or -4, or -28, or -35, and so on. And there are some influenzas that are also a threat. So, I hope we come away with the fundamental message that strong public health support must be a fundamental part of not just American society, but global society.
“I’d say our science has accelerated 10 years beyond where we would be without COVID. So, I think that’s the good news.”
John swartzerg
Reingold: I would say I do think the pandemic will accelerate and augment some improvements to public health infrastructure, particularly on the technology end—better computers and so forth. And I think that’s to the good, but unlike many countries, health care is primarily a state rather than a federal matter in the United States, and we’re going to continue to be a very fractured country in that regard. I don’t see much interest in many states, including California, in funding health care at a robust and ongoing level. So I don’t know how that will turn out.
Swartzberg: On the other hand, we’re also seeing what’s been termed the Fauci effect: Medical school applications are way up, and applicants are expressing a tremendous interest in public health. A lot of people want to matriculate into public health, so there’s certainly a growing societal awareness of its importance.
Riley: We’ve had a huge increase in the number of applicants to our infectious disease Ph.D. program—I think it’s doubled over the last year.
Reingold: As is true with every disease, with a few exceptions, COVID has clearly pointed to the social class disparities in health care and health outcomes. Often that appears in the form of race and ethnicity, but it remains largely a question of economics and social class in the absence of a national health care system. And I don’t think that’s going to be fixed anytime soon, frankly.
Swartzberg: I’m going to put a positive spin here: I think COVID has accelerated our basic knowledge about biological sciences in general and infectious diseases in particular. Just guessing, I’d say our science has accelerated 10 years beyond where we would be without COVID. So, I think that’s the good news.
How concerned are you that a virus worse than SARS-CoV-2 could be coming down the pike? And how ready are we socially and medically for something like that?
Riley: I think COVID is a wake-up call for the whole world. This is the third coronavirus pandemic that we’ve seen in this century—and obviously, this isn’t going to be the last one. But until recently, we weren’t really worried much about coronaviruses. The first one, I think, was discovered in the 1960s, and they were typically associated with common colds and mild respiratory illnesses. But SARS, in 2003, came out of the blue—no one expected a coronavirus to do anything like that. And then it disappeared on its own after six months. We know these viruses circulate in animal reservoirs, and as we encroach on wild habitats, people can get infected, and you can eventually get something that’s transmitted person-to-person. And if it’s a highly virulent virus, you can get a pandemic along the lines of what we’re seeing now—or worse.
Reingold: So if “it” turns out to be something like smallpox or Ebola, are we in trouble? Yes. Or if you have [a coronavirus] as equally transmissible as SARS-CoV-2 but instead of causing a tiny fraction of the people to become sick or die, it’s more like 30 percent, then sure, it’s going to be very serious. But anyone who says they can predict when something like that is going to happen—they’re just guessing. I don’t care if they’re a Nobel Prize–winning biologist or animal ecologist or epidemiologist or infectious disease specialist, it’s all a guess.
Swartzberg: But we should absolutely plan for it.
Reingold: I agree with that.
Swartzberg: From my perspective, we were all born in a very blessed time in human history. From the earliest civilizations, there were endemic diseases that were killing people right and left, all the time. But the world we’ve lived in for the past few generations has been far safer. And perhaps it will turn out that this has been the exception. Maybe the future will be more like the world we lived in before modern medicine, including vaccines. I know it’s anathema to think that, but it could be the case.
You mentioned the importance of better funding for public health, but what does that look like? What can we do with more money?
Reingold: Some of it is just about having the appropriate number of people with appropriate training and paying them salaries that are reliable and competitive. You have to think about the needs at the state and local levels. Some of it is maintenance, some of it is better technology and better communication. And it’s also about consistency—just ensuring that state and local infrastructure is reliable, that it’s going to always be there.
Swartzberg: I agree, and I’d just double underline “consistency.” It doesn’t do any good to just fund a five-year program. You need to have people in positions who understand the system, and you need to have them long term: people who’ve had 20 years of experience, so they understand what to do when the next pandemic hits. You can’t depend on filling in with new hires when there’s a crisis.
Riley: When I worked at the Centers for Disease Control, I was in a program that was essentially an intelligence service. We were sent out to investigate outbreaks. I was sent out all over the world, part of a tiny army of people who do that kind of work. I think it’s time we greatly expanded that program, including domestically. We need this kind of resource at the state level, not just the federal level. I think this pandemic reveals that our current public health system is totally ineffective—but we now have the opportunity to do something about it.
In a more positive light, I think the CDC will regain its reputation at some point. In the past, the CDC was highly respected and recognized as an important public health organization by a large segment of the U.S. population. They did a very good job with the 2001 anthrax scare and the emergence of the Zika virus, for example. Sometimes the problem is that when there’s nothing going on, the CDC and other public health organizations are invisible, but the reason they’re invisible is because they’re doing their jobs. Then when something happens, the response can be negative.
Reingold: A really fundamental problem is that there is no political support—or even support in the general population—to empower public health to do the important and necessary things that would allow it to effectively address or avoid pandemics.
And does that imply ensuring that government has the power to enforce mandates?
Reingold: Mandates are part of it. There are other ways to get things done, but at the end of the day, public health is intrinsically political, and laws and enforcement are a part of that entire process. Thankfully, SARS-CoV-2 is not preferentially killing young adults and children. But do you think the response would be radically different if that were the case?
My friends in gerontology and geriatrics have a real concern about ageism with this pandemic–the attitude that, “You’re old and we really don’t care if you die or not.”
Arthur Reingold
Swartzberg: You know, I spoke to some young people recently. They were in their late teens, and their take was this doesn’t seem so serious, let’s just get it and get it over with. And that struck me as analogous to our approach as a nation—that as long as we’re protected, as long as we’re vaccinated and get the number of infections down, we’re okay. And we’re seeing that somewhat selfish approach to the pandemic breaking along age differentials as well. They’re wondering why they should curtail things they want to do to protect other people. It points to still another fracture line in our society, this one based on age.
Reingold: My friends in gerontology and geriatrics have a real concern about ageism with this pandemic—the attitude that, “You’re old and we really don’t care if you die or not,” or, “Too bad for you, you’ve had a good life, so get over it.” And that outrages my friends, who are committed to taking care of all people of all ages. You know, this country mobilized itself to get rid of polio because there were children paralyzed and in iron lungs. But the fact is that only 1 in 200 children infected with the poliovirus developed paralysis. The other 199 were either asymptomatic or had very mild or limited illnesses. But we went to a great deal of trouble to prevent those incredibly uncommon but very serious illnesses because they were horrible, and we weren’t willing to say, “Well, let’s just let the poliovirus rip through the population and get it over with.”
Glen Martin is a longtime contributor to California.